Dear Friend,
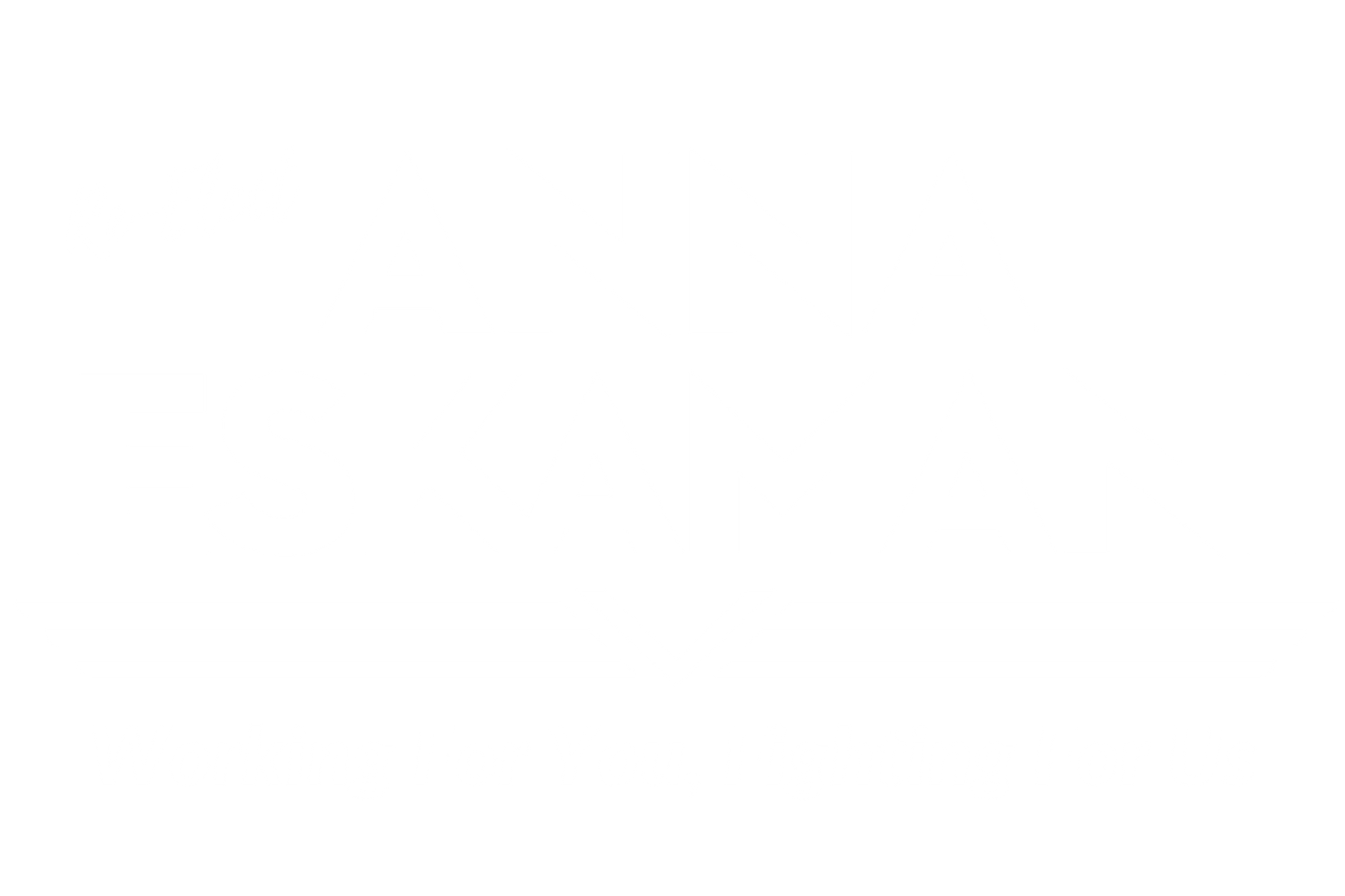
Almost a quarter of Florida residents — some 5.5 million people — pay for medical treatment through Medicaid, a federal government program for low-income families.
But close to a million of those could be thrown off the program over the coming year as the state has begun the first purge of its Medicaid rolls since the start of the pandemic in 2020.
Enrollment in Florida’s Medicaid program ballooned by 1.7 million people, including 500,000 children, during the public health emergency when the federal government paid states to keep residents enrolled no matter their situation.
Those payments end this year, and the Florida Department of Children and Families plans to review the eligibility of almost 5 million recipients, removing any who no longer qualify for the benefit.
The department has already identified around 900,000 recipients it said were no longer eligible based on 2022 income data. Another 850,000 recipients had not responded to requests from the state for details about their income.
Local nonprofits and health care agencies fear the result will be an unprecedented wave of hundreds of thousands of Floridians losing coverage, causing the state’s uninsured rate to rocket and leaving many residents, including children, with no access to medical care.
We want to make sure you are aware of this change, and provide you with information in case you are impacted. A few weeks ago we hosted a virtual event with Primary Care Access Network focused on this topic that you can find here.
Below are additional detail, most of which are pulled from this Tampa Bay Times article.
Why is this happening now?
The Families First Coronavirus Response Act, passed in the early days of the pandemic, required states to provide continuous Medicaid coverage to recipients even if they became ineligible. In return, the federal government increased its share of medical bills by about 6%. The measure was intended to ensure low income families could afford medical treatment during the public health emergency. With that emergency coming to an end, Congress set March 31 as the end date for continuous coverage. The Centers for Medicare & Medicaid Services is giving states up to a year to transition back to normal Medicaid operations.
Why would families stop being eligible for Medicaid?
Families can become ineligible through a change in income such as a new job or a pay raise. Florida has among the strictest eligibility rules for Medicaid in the nation. It is also one of 10 states not to take advantage of Medicaid expansion, a provision of the Affordable Care Act that provides incentives to states that expand the program to more low-income families.
Florida’s Medicaid program covers children ages 5 and younger in households that make $33,408 or less and older children whose parents make up to $31,795. There is no coverage for parents who earn more than $7,000 per year, and adults with no children are ineligible no matter how little they earn.
How will I know if I’m losing my Medicaid coverage?
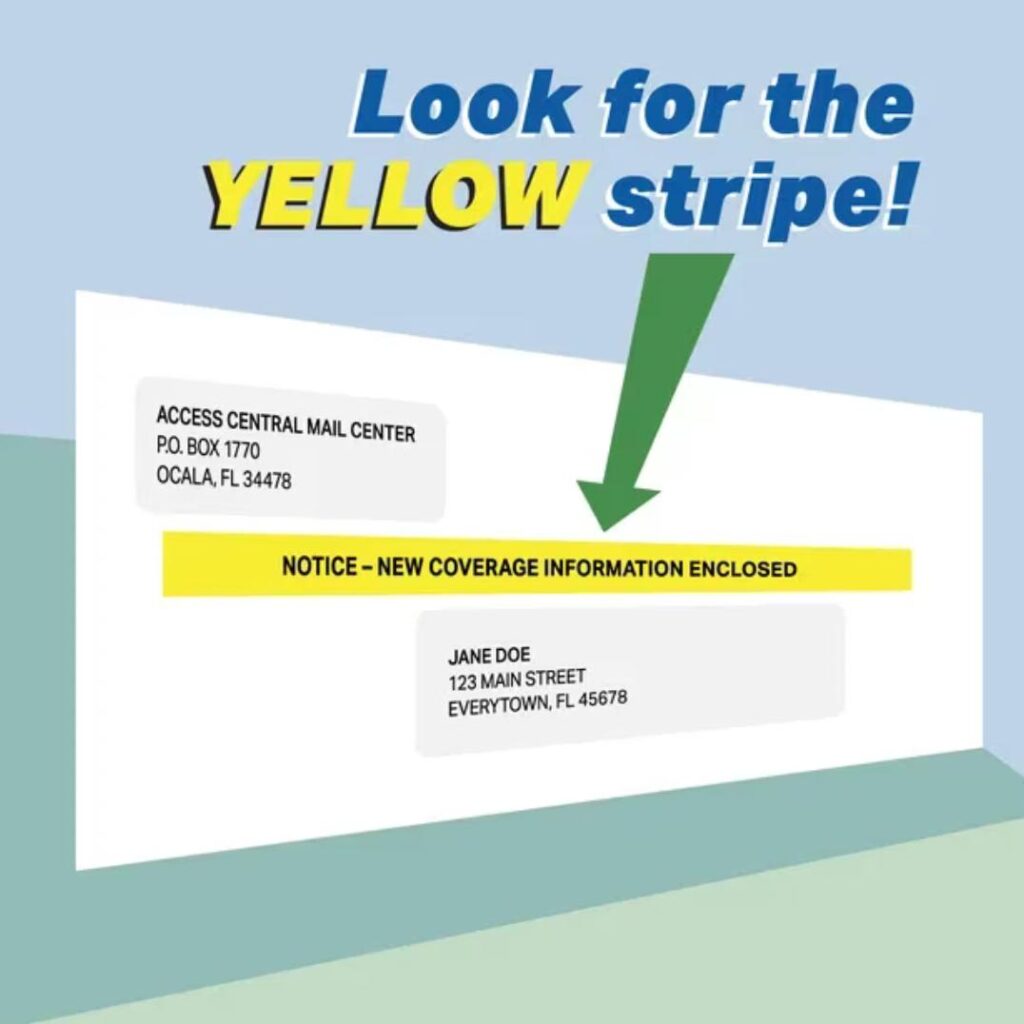
Recipients are advised to make sure their contact details are up to date by logging onto their myaccess account. They also should look for an envelope with a yellow stripe or an email seeking information that will be sent 45 days prior to a recipient’s renewal date. Those whom the state cannot renew because they lack up-to-date income information or because they are deemed ineligible will receive a 45-day notice by letter or email. They will then have 90 days to reapply if they believe they are still eligible.
Those losing coverage who may be eligible for other programs will automatically be referred to Florida KidCare, the Medically Needy Program and other subsidized federal health care programs, according to the state’s plan.
How will the state manage this transition?
The Florida Department of Children plans to add 137 call center agents to deal with an anticipated surge in calls, according to a 43-page plan it released earlier this year. The first residents to be reviewed and potentially removed will be the 900,000 whose income data showed they earn too much to qualify for Medicaid. Residents who have not responded to requests for income information will also be prioritized in the review.
Where can I get help or more information?
Residents seeking more information can log onto the Florida Department of Children and Families website or call the department at 850-300-4323.
More extensive help is available locally through a collaboration between the Family Healthcare Foundation, BayCare Health System, Tampa General Hospital, Evara Health and Premier Community Healthcare Group, which is providing 35 navigators to assist residents worried about losing coverage. The service is free and confidential. Residents can reach out online or by calling 813-995-7005.
Central Floridians can also reach out to Covering Central Florida.